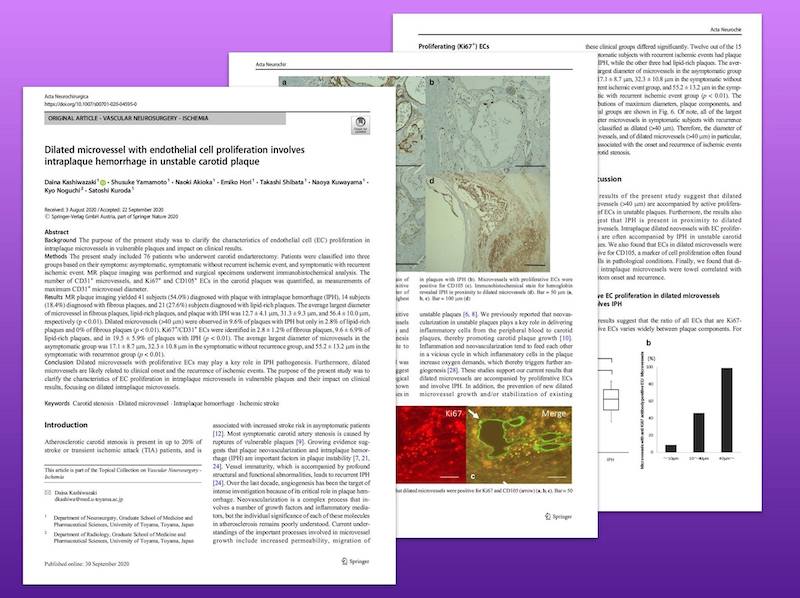
当科の柏崎大奈先生の論文が「Acta Neurochir (Wien)」誌に掲載されました。今回の新たな頚動脈狭窄症の研究は、頚動脈プラーク内に形成された幼若な血管の拡張と血管内皮前駆細胞の増殖が盛んなほど、プラーク内出血、ひいては脳梗塞などの脳血管イベントが誘発されやすいことを初めて明らかにしました。全身そして局所の血管病変に潜在する慢性炎症がこれら負のスパラルの温床になっていると、われわれは考えています。
A Voyage to Depth of Neuroscience Vol. 76
Kashiwazaki D, Yamamoto S, Akioka N, Hori E, Shibata T, Kuwayama N, Noguchi K, Kuroda S.
Dilated microvessel with endothelial cell proliferation involves intraplaque hemorrhage in unstable carotid plaque,
Acta Neurochir (Wien). 2020 Sep 30. doi: 10.1007/s00701-020-04595-0. Online ahead of print.
Abstract
Background: The purpose of the present study was to clarify the characteristics of endothelial cell (EC) proliferation in intraplaque microvessels in vulnerable plaques and impact on clinical results.
Methods: The present study included 76 patients who underwent carotid endarterectomy. Patients were classified into three groups based on their symptoms: asymptomatic, symptomatic without recurrent ischemic event, and symptomatic with recurrent ischemic event. MR plaque imaging was performed and surgical specimens underwent immunohistochemical analysis. The number of CD31+ microvessels, and Ki67+ and CD105+ ECs in the carotid plaques was quantified, as measurements of maximum CD31+ microvessel diameter.
Results: MR plaque imaging yielded 41 subjects (54.0%) diagnosed with plaque with intraplaque hemorrhage (IPH), 14 subjects (18.4%) diagnosed with fibrous plaques, and 21 (27.6%) subjects diagnosed with lipid-rich plaques. The average largest diameter of microvessel in fibrous plaques, lipid-rich plaques, and plaque with IPH was 12.7 ± 4.1 μm, 31.3 ± 9.3 μm, and 56.4 ± 10.0 μm, respectively (p < 0.01). Dilated microvessels (>40 μm) were observed in 9.6% of plaques with IPH but only in 2.8% of lipid-rich plaques and 0% of fibrous plaques (p < 0.01). Ki67+/CD31+ ECs were identified in 2.8 ± 1.2% of fibrous plaques, 9.6 ± 6.9% of lipid-rich plaques, and in 19.5 ± 5.9% of plaques with IPH (p < 0.01). The average largest diameter of microvessels in the asymptomatic group was 17.1 ± 8.7 μm, 32.3 ± 10.8 μm in the symptomatic without recurrence group, and 55.2 ± 13.2 μm in the symptomatic with recurrence group (p < 0.01).
Conclusion: Dilated microvessels with proliferative ECs may play a key role in IPH pathogenesis. Furthermore, dilated microvessels are likely related to clinical onset and the recurrence of ischemic events. The purpose of the present study was to clarify the characteristics of EC proliferation in intraplaque microvessels in vulnerable plaques and their impact on clinical results, focusing on dilated intraplaque microvessels.