近年、わが国でも急速に増加しつつある頚部内頚動脈狭窄症ですが、その病態には未だに不明の部分が多いのが現状です。今回、われわれは、頚動脈内膜剥離術(CEA)にて摘出した頚動脈プラーク病変を詳細に観察することで、骨髄から末梢血に動員された内皮前駆細胞(endothelial progenitor cell; EPC)が頚動脈プラークの増大、血管新生、プラーク内出血、脆弱性に深く関与していることを明らかとしました。当科の柏崎大奈先生がその成果をJournal of Neurosurgery (JNS)に発表してくれました。今後、頚部内頚動脈狭窄症に対する新たな治療戦略の構築や創薬を進める上で有用な情報となることを期待しています。
A Voyage to Depth of Neuroscience Vol. 25
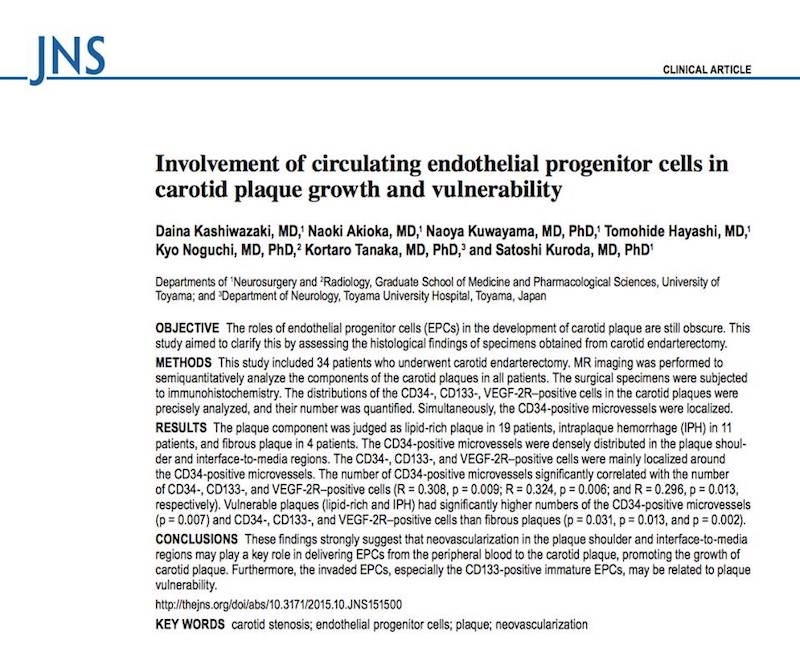
Kashiwazaki D, Akioka N, Kuwayama N, Hayashi T, Noguchi K, Tanaka K, Kuroda S:
Involvement of circulating endothelial progenitor cells in carotid plaque growth and vulnerability.
J Neurosurg 2016 Feb 12 [Epub ahead of print]
http://www.ncbi.nlm.nih.gov/pubmed/26871204
Abstract
OBJECTIVE The roles of endothelial progenitor cells (EPCs) in the development of carotid plaque are still obscure. This study aimed to clarify this by assessing the histological findings of specimens obtained from carotid endarterectomy. METHODS This study included 34 patients who underwent carotid endarterectomy. MR imaging was performed to semiquantitatively analyze the components of the carotid plaques in all patients. The surgical specimens were subjected to immunohistochemistry. The distributions of the CD34-, CD133-, VEGF-2R-positive cells in the carotid plaques were precisely analyzed, and their number was quantified. Simultaneously, the CD34-positive microvessels were localized. RESULTS The plaque component was judged as lipid-rich plaque in 19 patients, intraplaque hemorrhage (IPH) in 11 patients, and fibrous plaque in 4 patients. The CD34-positive microvessels were densely distributed in the plaque shoulder and interface-to-media regions. The CD34-, CD133-, and VEGF-2R-positive cells were mainly localized around the CD34-positive microvessels. The number of CD34-positive microvessels significantly correlated with the number of CD34-, CD133-, and VEGF-2R-positive cells (R = 0.308, p = 0.009; R = 0.324, p = 0.006; and R = 0.296, p = 0.013, respectively). Vulnerable plaques (lipid-rich and IPH) had significantly higher numbers of the CD34-positive microvessels (p = 0.007) and CD34-, CD133-, and VEGF-2R-positive cells than fibrous plaques (p = 0.031, p = 0.013, and p = 0.002). CONCLUSIONS These findings strongly suggest that neovascularization in the plaque shoulder and interface-to-media regions may play a key role in delivering EPCs from the peripheral blood to the carotid plaque, promoting the growth of carotid plaque. Furthermore, the invaded EPCs, especially the CD133-positive immature EPCs, may be related to plaque vulnerability.