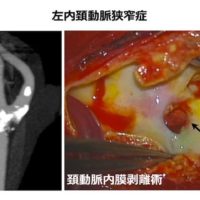
近年、一過性脳虚血発作(TIA)と脳梗塞とを区別せず、急性脳血管症候群(acute cerebrovascular syndrome; ACVS)という一つの疾患概念として捉えて、診断や治療を論じるべきであると考えられています。これまでは頚動脈狭窄症がこのACVSを引き起こすメカニズムを症例ごとに明確にすることは困難でした。
今回、当院でのデータをもとに、MRIプラーク・イメージングと脳SPECTの所見を複合的に組み合わせることで、ACVSの発生メカニズムを明らかにできることを米国脳神経外科コングレス機関誌「Neurosurgery」に報告させていただきました。
この研究は当科の柏崎大奈先生が中心となって実施しましたが、神経内科の田中耕太郎教授、放射線科の野口 京教授のご助力のおかげで完遂することができました。この場をお借りして御礼申し上げます。
詳細は以下をご参照下さい。
Kashiwazaki D, Akioka N, Kuwayama N, Noguchi K, Tanaka K, Kuroda S: Pathophysiology of acute cerebrovascular syndrome (ACVS) in patients with carotid artery stenosis: A MRI/SPECT study. Neurosurgery 2015 Jan 23 [Epub ahead of print]
http://www.ncbi.nlm.nih.gov/pubmed/25621983
A Voyage to Depth of Neuroscience Vol. 19 Pathophysiology of acute cerebrovascular syndrome (ACVS) in patients with carotid artery stenosis: A MRI/SPECT study.
BACKGROUND:The mechanisms underlying acute cerebrovascular syndrome in patients with carotid artery stenosis remain unclear.
OBJECTIVE: To assess the relationships among infarct localization, hemodynamics, and plaque components.
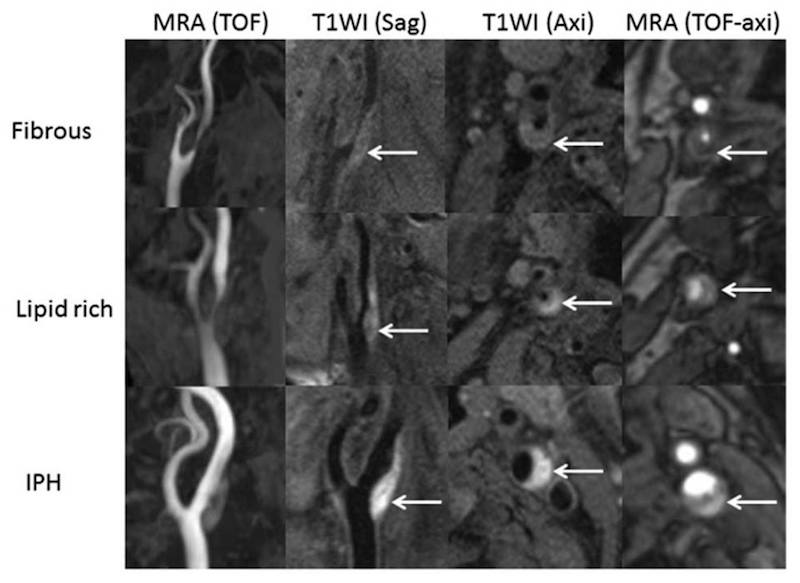
METHODS: This prospective study included 38 patients with acute cerebrovascular syndrome resulting from ipsilateral carotid artery stenosis. Cerebral infarct localization was categorized into 3 patterns (cortical, border zone, and mixed pattern). Carotid plaque components were evaluated with T1-weighted magnetic resonance imaging and time-of-flight imaging. Cerebral blood flow (CBF) and cerebrovascular reactivity (CVR) were also quantified.
RESULTS: Infarcts were identified in 38 patients with the use of diffusion-weighted magnetic resonance imaging. On the basis of the assessment of hemodynamics, the cortical pattern was seen in 18 of 21 patients with type 1 ischemia (normal CBF, normal CVR), whereas the mixed pattern was seen in 2 patients with type 2 ischemia (normal CBF, impaired CVR) and 12 of 15 patients with type 3 ischemia (impaired CBF, impaired CVR). The plaque components were categorized into fibrous (4 patients), lipid-rich (14 patients), and intraplaque hemorrhage (IPH; 20 patients). Of the patients with fibrous plaque, 2 had border-zone and 2 had mixed-pattern infarcts. Of the patients with lipid-rich plaque, 7 had cortical and 6 had mixed-pattern infarcts. Of patients with intraplaque hemorrhage, 11 had cortical and 9 had mixed-pattern infarcts.
CONCLUSION: Cortical infarction occurs as a result of vulnerable plaque. Reduced cerebral perfusion induces border-zone infarction. Both factors are implicated in mixed-pattern infarction. Developments in noninvasive diagnostic modalities allow us to explore the mechanisms behind acute cerebrovascular syndrome in carotid artery stenosis and to determine the ideal therapies.