当科の柏崎大奈先生の論文「不安定プラークを有する症候性軽度(<50%)頚動脈狭窄症に対する頚動脈内膜剥離術の効果」がWorld Neurosurgery誌に掲載されました。
症候性軽度(<50%)頚動脈狭窄症の患者さんに対しては、従来の大規模臨床試験の結果、これまで内科治療を実施することが推奨されてきました。しかし、一部の患者さんは最適な内科治療にもかかわらず脳梗塞を再発することが広く知られつつあります。特に、MRIのスピンエコーT1強調画像にて高信号を呈する不安定プラークを有する症例ではこの頻度が低くなく、狭窄率のみならず、プラークの性状に基づいた治療指針の確立が必要となりつつあります。この研究では、上記のような症例に対して頚動脈内膜剥離術を実施すると、長期予後を含めた治療成績が大変良好であることを示しました。
この研究は、現在、宇野昌明先生(川崎医科大学)、小笠原邦昭先生(岩手医科大学)と共同で実施中の多施設共同臨床研究「プラーク性状に基づいた内頚動脈軽度狭窄症(50%未満)の予後と外科治療の意義(MUSIC研究; UMIN000023635)」と同様の理論的背景を有するものです。
A Voyage to Depth of Neuroscience Vol. 53
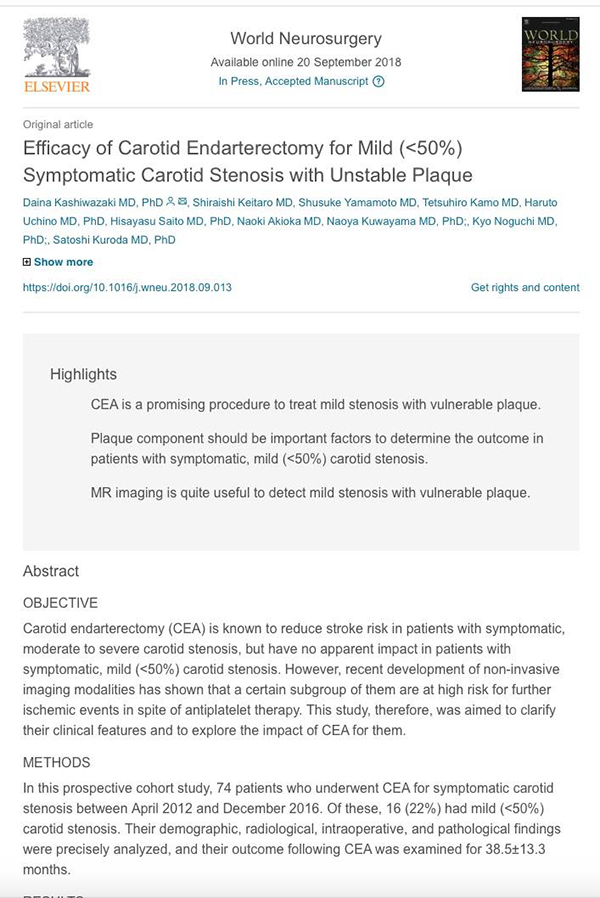
One of our staff, Dr. Daina Kashiwazaki published a paper on carotid endarterectomy for medical treatment-resistant patients with mild (<50%) carotid stenosis complicated by unstable plaque.
Kashiwazaki D, Keitaro S, Yamamoto S, Kamo T, Uchino H, Saito H, Akioka N, Kuwayama N, Noguchi K, Kuroda S.
World Neurosurgery 2018 Sept 29. [Epub ahead of print]
Efficacy of Carotid Endarterectomy for Mild (<50%) Symptomatic Carotid Stenosis with Unstable Plaque.
Abstract
OBJECTIVE:
Carotid endarterectomy (CEA) is known to reduce stroke risk in patients with symptomatic, moderate to severe carotid stenosis, but have no apparent impact in patients with symptomatic, mild (<50%) carotid stenosis. However, recent development of non-invasive imaging modalities has shown that a certain subgroup of them are at high risk for further ischemic events in spite of antiplatelet therapy. This study, therefore, was aimed to clarify their clinical features and to explore the impact of CEA for them.
METHODS:
In this prospective cohort study, 74 patients who underwent CEA for symptomatic carotid stenosis between April 2012 and December 2016. Of these, 16 (22%) had mild (<50%) carotid stenosis. Their demographic, radiological, intraoperative, and pathological findings were precisely analyzed, and their outcome following CEA was examined for 38.5±13.3 months.
RESULTS:
Of these 16 patients, 12 had already been treated with antiplatelets against previous ischemic cerebrovascular or coronary artery diseases. Plaque MR imaging revealed that all patients had the vulnerable plaque, including lipid-rich plaque (n=6) and intraplaque hemorrhage (IPH; n=10). Intraoperative observations confirmed it. Histological analysis revealed that inflammatory cells and fragile angiogenesis were widely found in the specimen. Only one patient experienced transient (<30 days) neurological deficits after CEA, but none of them repeated cerebrovascular events during follow-up periods.
CONCLUSIONS:
There are not a few patients who are at high risk for subsequent ischemic events because of vulnerable plaque in spite of mild (<50%) carotid stenosis. MR imaging is quite useful to non-invasively detect such vulnerable plaques. CEA is a promising procedure to treat them.