A Voyage to Depth of Neuroscience Vol. 78
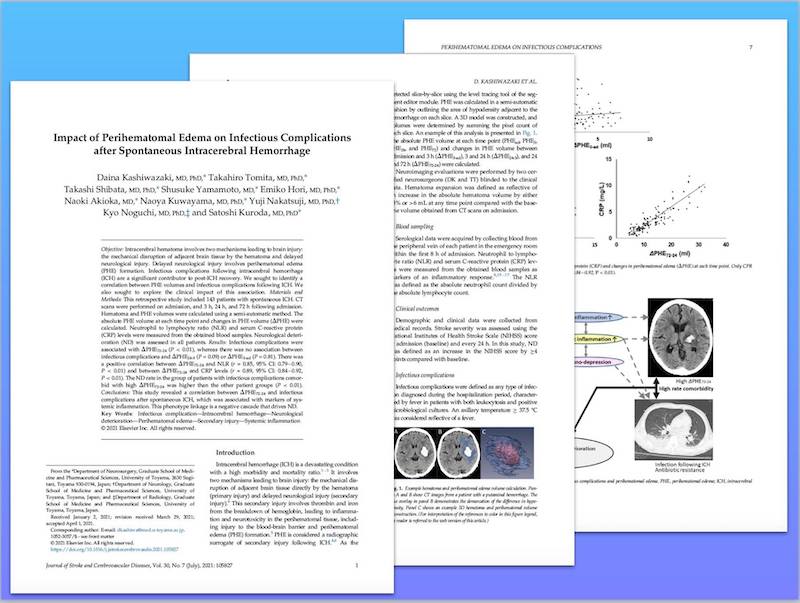
当科の柏崎大奈先生の論文がJournal of Stroke and Cerebrovascular Diseases誌に掲載されました。脳出血周囲には脳浮腫が出現することは誰もがよく知っている事実です。しかし、今回の研究によって、発症24時間後から72時間後にかけて脳浮腫増大の程度が高度であるほど、肺炎などの感染症が多く、白血球のうち好中球が占める割合が高く、さらに炎症性タンパク質であるCRPが高値であるとともに、神経症状の悪化に関与していることが初めて明らかになりました。
脳出血に続発する脳浮腫が脳内に留まらず、全身の炎症を惹起するとともに免疫機能にも影響を及ぼすことで易感染性を招来していることが示唆されます。
Kashiwazaki D, Tomita T, Shibata T, Yamamoto S, Hori E, Akioka N, Kuwayama N, Nakatsuji Y, Noguchi K, Kuroda S:
Impact of Perihematomal Edema on Infectious Complications after Spontaneous Intracerebral Hemorrhage.
J Stroke Cerebrovasc Dis. 2021 Apr 28;30(7):105827. doi: Online ahead of print.
Abstract
Objective: Intracerebral hematoma involves two mechanisms leading to brain injury: the mechanical disruption of adjacent brain tissue by the hematoma and delayed neurological injury. Delayed neurological injury involves perihematomal edema (PHE) formation. Infectious complications following intracerebral hemorrhage (ICH) are a significant contributor to post-ICH recovery. We sought to identify a correlation between PHE volumes and infectious complications following ICH. We also sought to explore the clinical impact of this association.
Materials and methods: This retrospective study included 143 patients with spontaneous ICH. CT scans were performed on admission, and 3 h, 24 h, and 72 h following admission. Hematoma and PHE volumes were calculated using a semi-automatic method. The absolute PHE volume at each time point and changes in PHE volume (ΔPHE) were calculated. Neutrophil to lymphocyte ratio (NLR) and serum C-reactive protein (CRP) levels were measured from the obtained blood samples. Neurological deterioration (ND) was assessed in all patients.
Results: Infectious complications were associated with ΔPHE72-24 (P < 0.01), whereas there was no association between infectious complications and ΔPHE24-3 (P = 0.09) or ΔPHE3-ad (P = 0.81). There was a positive correlation between ΔPHE72-24 and NLR (r = 0.85, 95% CI: 0.79-0.90, P < 0.01) and between ΔPHE72-24 and CRP levels (r = 0.89, 95% CI: 0.84-0.92, P < 0.01). The ND rate in the group of patients with infectious complications comorbid with high ΔPHE72-24 was higher than the other patient groups (P < 0.01).
Conclusions: This study revealed a correlation between ΔPHE72-24 and infectious complications after spontaneous ICH, which was associated with markers of systemic inflammation. This phenotype linkage is a negative cascade that drives ND.